With the Ontario government moving towards implementing pharmacist-led minor ailment services that would allow pharmacists to prescribe for a number of common conditions, BC will soon be the only province without such services.
Is pharmacist prescribing for minor ailments needed?
Healthcare costs in BC are mounting, with nearly half our provincial budget spent towards it.1 While there is a growing need for increased access to healthcare, the current system is unsustainable. For instance, it is estimated that 700,000 British Columbians are without a family doctor.2
However, simply having a family physician does not mean you have adequate access to primary care. A majority of Canadians (68%) actually skip seeing a doctor due to long wait-times, timeliness, and other barriers.3 Over half of patients (54%) are unable to find an appointment with their physician on the same or following day, and many (56%) identify a difficulty finding after-hour care, such as evenings, weekends, and holidays.4
In response to these mounting concerns, BC Provincial Health Minister Dix made it his top priority to establish urgent family care centers to improve access to primary care. However, utilizing pharmacists to the full scope of our knowledge, skills and abilities would also expand access to primary care. That is why Ontario Premier Doug Ford recently announced in his budget release that pharmacists will have prescribing authority for minor ailments, which was identified as a “basic change” to save patients’ time and money.
Why pharmacists?

Pharmacists can help meet the growing demand for convenient, accessible and cost-effective healthcare. Pharmacists are the most accessible healthcare professionals, with over 41,000 licensed pharmacists working in 10,000 pharmacies across Canada in convenient locations.5 Pharmacists are available outside of the usual GP working hours, such as during evenings and on weekends and holidays – times where access to primary care is significantly reduced.
Pharmacists have the knowledge and skills to assess and manage minor ailments. In fact, pharmacists across the country have already been doing so for a long time when they make over-the-counter (OTC) medication recommendations. Furthermore, almost all Canadians (93%) trust pharmacists to provide advice on managing minor ailments.6
Related: 7 reasons you should be proud to be a pharmacist
What is the rest of Canada doing?
Although the scope for pharmacist prescribing differs between the provinces, currently 8 of the 10 Canadian provinces allow pharmacist prescribing for minor ailments.7

Alberta led the way with pharmacist prescribing in 2007, with Nova Scotia and Saskatchewan following suite. Since then, New Brunswick, Prince Edward Island, Newfoundland, Manitoba and Quebec also have implemented pharmacist-led minor ailment services. And finally, earlier this month the Ontario government announced that it intends to give pharmacists prescribing authority for minor ailments. Once in place, BC will be the only province in Canada without pharmacist prescribing authority for minor ailments.
Pharmacist prescribing for minor ailments is successful
The implementation of pharmacist-led minor ailment services across Canada has been successful. A Saskatchewan study showed that the condition pharmacists treated improved in 81% of patients.8 Patients were also satisfied with the service, with only 6% feeling a physician would have been more thorough.8

In New Brunswick, pharmacist prescribing for uncomplicated UTIs has been applauded as a means to reducing unnecessary ER visits. A study found that most (94.5%) patients with a UTI managed by a pharmacist achieved clinical cure.9 Conversely, adverse drug reactions, most commonly transient GI side effects, were reported in only 7% of patients.9
Pharmacists can divert care of minor ailments from other areas of healthcare
It has been estimated that 18-40% of a family physician’s workload and 5% of emergency room consultations are for minor ailments.10 In fact, nearly half (47%) of patients who visited the ER in the previous year said their condition could have been treated by their regular place of care (family physician or walk-in clinic) if the doctor had been available.11

Pharmacists can help alleviate the workload of family physicians and prevent unnecessary visits to the ER. After the implementation of pharmacist-led minor ailment services in Scotland, there was a 38% transfer from family physicians to pharmacists for those conditions.12 While this data has not yet been directly researched in Canada, provincial studies evaluating pharmacist-led minor ailment services in Canada have identified a similar trend. For instance, a study in Nova Scotia identified that 87% of patients would have seen a physician if the pharmacist service was unavailable, 9% would have visited the ER, and 10% would not have sought immediate care.13
Pharmacists can save the healthcare system money
Based on an estimate that BC physicians bill $95 million minimum annually for minor ailments, the BC Pharmacy Association calculated that pharmacist-led minor ailment services has the potential to save the BC healthcare system approximately $32 million.10
Cost savings are usually estimated by calculating the savings of diverting care from family physicians, who bill on average $48.11 per service.14 For example, a 1996 study estimated that pharmacists make around 15 million OTC interventions per year (at that time).15 If even a quarter of those patients chose to seek a physician instead, it would have meant an extra $169 million in physician billing.15

Cost savings has been proven in other provinces. For instance, it was found that for every dollar spent on pharmacists’ prescribing for minor ailments in Saskatchewan, including the government-covered $18 pharmacist fee for the service, the province saved $2.15 in direct healthcare costs and indirect costs.16
This financial benefit is in addition to the value of optimizing physicians’ time, reducing overall wait times, and increasing access to primary care.
What’s next for pharmacist prescribing in BC?
The College of Pharmacists of BC has submitted a proposal for Certified Pharmacists Prescribing (CPP) to the BC Ministry of Health for consideration. A Certified Pharmacist prescriber would be able to independently start, change, adjust, and stop a patients’ medication treatment in collaboration with other prescribing healthcare professionals.
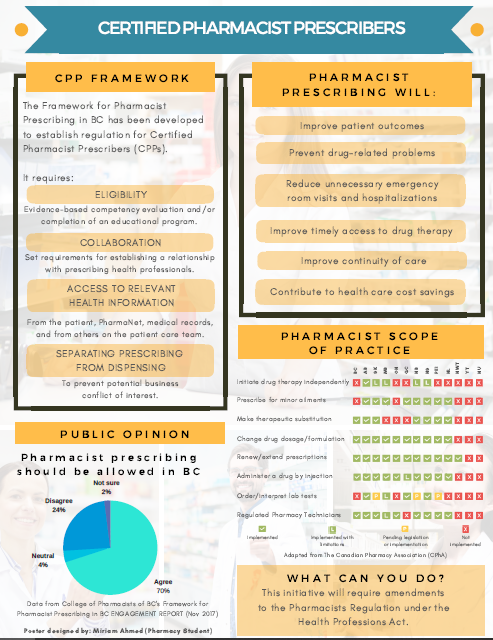
However, the CPP proposal has been criticized by some, such as the BC Pharmacy Association, who feel that the framework is too narrow in restricting pharmacist prescribing to only within collaborative practice. They advocate for pharmacist-led minor ailment services instead to increase patient access to primary care, particularly in remote and rural communities.
BC is currently awaiting a decision from the Ministry of Health regarding the Certified Pharmacist Prescriber proposal.
Moving forward – what are your thoughts?
The BC healthcare system is in need of cost-effective alternatives to increase access to primary care. The implementation of pharmacist minor ailment services in BC would not only reduce wait times for patients to see a healthcare provider and save the healthcare system millions, but would also ensure that every British Columbian has equal access to primary care in a timely and effective manner.
Do you agree with implementing pharmacist minor ailment services in BC? Leave a comment below with your thoughts!
References
- Canadian Institute for Health Information (CIHI): National Health Expenditure Trends, 1975 to 2014 (October 2016).
- Statistics Canada: Primary health care providers, 2016 (September 2017).
- Ipsos: Seven in 10 Canadians (68%) have skipped seeing a doctor due to long wait times, timeliness or other barriers (January 2017).
- Health Council of Canada: Where you live matters: Canadian views on health care quality (January 2014).
- National Association of Pharmacy Regulatory Authorities (NAPRA): National Statistics (January 2019).
- Abacus Data: Pharmacists in Canada (March 2018).
- Canadian Pharmacists Association: Pharmacists’ Expanded Scope of Practice (March 2019).
- Mansell et al. Evaluating pharmacist prescribing for minor ailments. International Journal of Pharmacy Practice. 2015; 23(2):95-101.
- Beahm et al. Outcomes of Urinary Tract Management by Pharmacists (RxOUTMAP): A study of pharmacist prescribing and care in patients with uncomplicated urinary tract infections in the community. Canadian Pharmacists Journal. 2018; 151(5):305-314.
- British Columbia Pharmacy Association (BCPhA): Clinical Service Proposal Treatment of Minor Ailments (March 2013).
- Health Council of Canada: How do Canadians rate the health care system? (November 2010).
- Wagner et al. Changing patient consultation patterns in primary care: an investigation of uptake of the Minor Ailments Service in Scotland. Health Policy. 2011; 99(1):44-51.
- Pharmacy Association of Nova Scotia (PANS): Evaluation of the Provision of Minor Ailment Services in the Pharmacy Setting Pilot Study (October 2013).
- Canadian Institute for Health Information (CIHI): Physicians in Canada (February 2017).
- Taylor and Joubert. Pharmacist-led minor ailment programs: a Canadian perspective. International Journal of General Medicine. 2016; 9:291-302.
- Rafferty et al. Costs and savings association with a pharmacists prescribing for minor ailments program in Saskatchewan. Cost Effectiveness and Resource Allocation. 2017; 15:3.
I do not agree with Pharmacist prescribing and this is why. I broke my back and had surgery in 2001 I have manger just fine until now. Now I have discs that are gone not degenerating gone, and I have managed that pain with Tylenol 1 but the Pharmacist in Chetwynd at the IDA drug store seems to think that my taking Tramadol/ ACET is better and actually said it is non addictive and we know that isn’t true. I had to get my doctor to prescribe the Tylenol 1’s which was 3×3 times a day this Pharmacist re wrote it to 1×3 because he said they are addictive even though I said I do not like the Tramadol because they get me high and I don’t like it as to where the T’1’s mange my pain with out getting me high, and the Tramadol is only for when the pain is really bad. I think that I know my body and my mind better than any one and this is not right and to me it sounds like they are trying to start the opioid epidemic here in Canada now. No I am not going to let this go and him changing my prescription is not right, to refuse one drug that is lower dose, one that a function normally on because I am not stoned out of my mind but say yes to the one that is to me more addictive and gets me stoned out of my mind to where I could hurt myself more is crap. So if that expertise we are all in trouble !!!
LikeLike